AI-powered Clinical Workflows
Designing a secure, AI-powered platform to help care teams close care gaps at scale, increase revenue, and reduce time spent chart hunting by 63%.

Capturing revenue and reducing burden on healthcare teams with Nimbus
ROLE
Principal Product Designer
Team
Sr. Principal Product Manager
2 Engineer Leads
5 Engineers across AI/ML, Full Stack, Systems Infrastructure, QA Testing
Data Analyst
User Researcher
SKILLS
AI prototyping, user research, product strategy zero to one product design, product analytics
OVERVIEW
The Digital Innovation Group (DIG) is a tech incubator at Providence that builds next-gen solutions for complex health systems. Nimbus is DIG’s first product designed and built for clinical workers.
Nimbus helps healthcare teams close care gaps efficiently at scale by integrating AI automation and workflow management.
project Impact
I designed an intelligent platform that enables teams to create, manage, and optimize their administrative and clinical workflows, resulting in:
98% match rate in finding patient data
63% time savings for caregiver teams
Up to $1.6 million in captured revenue

the problem
Manual workflows lead to administrative burden and caregiver burnout
In the healthcare system, ‘DIY’ workflows are inefficient. Spreadsheets, sticky notes, and multiple portals to complete a single task is the norm, taking time away from direct patient care.
Burnout and inefficiency cause staff turnover and higher costs. With 64% of workflows needing human input, administrative overhead is high. We identified 20+ use cases at Providence that could be improved and automated to reduce this burden.
Final Product
workflow management for healthcare
A new tool for care teams that seamlessly integrates patient data and saves time on chart hunting.
KEY FEATURES
AI data extraction makes finding the right data faster and easier
Nimbus integrates data from Electronic Health Records (EHRs), health insurance portals, and other sources into a single platform.
By using AI to unlock unstructured data like PDFs, scanned documents, and hand-written notes, which can constitute up to 80% of the patient record, caregivers can spend less time searching for data and more time on patient care.
Automating tasks for smoother collaboration and faster patient care
Nimbus automatically searches the patient record to find data that could close care gaps and surfaces them at the top of the list for caregivers. For patients with care gaps that can’t be closed, caregivers can quickly identify them and schedule health screenings.
Teams collaborate on Nimbus to review work, track statuses, leave notes, and smoothly hand off tasks, while also knowing that Protected Health Information (PHI) is handled safely and securely.
nimbus differentiator
Unstructured Data Analysis with AI
Most care gap tools focus on analytics, risk identification, or patient outreach. Nimbus stands apart by using AI to analyze unstructured EHR data — where up to 80% of clinical evidence for closing care gaps resides and where care teams spend the most time searching manually.
discovery research
Pain points in the current workflow
Working with our research team, I conducted user shadowing to understand the current workflow and identify major pain points in the process. Time studies revealed that:
52% of caregivers’ time was spent hunting for evidence in the EHR, looking through multiple tabs for lab results or procedures, reading past visit notes, reviewing scanned documents, and more.
15% of their time was spent verifying that the patient in the EHR matches the patient in the payer gap list
14% of their time was spent documenting their work in spreadsheets

design evolution
Creating a platform and design system that scales
I approached this as a systems design challenge, mapping how performance tracking, patient lists, and multi-role workflows would interconnect at scale. User testing validated the system thinking but showed we needed to phase development. I prioritized the highest-impact features for our V1 Proof of Concept, while designing flexible patterns that could evolve and ship incrementally based on user needs and engineering capacity.














learnings
Designing for focus: reduce the noise and make data actionable
Initial designs with content cards and tab navigation suffered from the same issue as Epic: too many tabs, hidden information, too much friction. I simplified navigation and surfaced AI-extracted evidence front and center, helping caregivers validate patient data faster and close care gaps more efficiently.
With only 7 months to launch and prove value, we had to ruthlessly prioritize. My initial designs outlined a full end-to-end vision for both Specialists and Managers, including list configuration, comments, and analytics. For the proof of concept, we focused on the Specialist flow first, while designing with a scalable, system-wide foundation in mind.
caregiver impact
Turning a tedious chart search into a single, effortless click
Before Nimbus
Caregivers had to sift through the entire patient list to find patients with evidence to close the gap, a time-consuming process that took on average of 4 hours per list.

After Nimbus
Nimbus finds patient with evidence and sorts them at the top of the list, making it much faster for caregivers to validate vs. manual chart hunting, resulting in 2.5 hours saved (63%).

business impact
Nimbus finds the right patient data, saves caregivers time, and has potential to generate millions for the health system.

Nimbus proved immediate value with a 98% patient match rate and 2.5+ hours saved per caregiver. By closing gaps faster, teams can increase overall closure rates and unlock higher performance bonuses, projected to generate up to $1.6 million in revenue across Providence’s payer contracts.
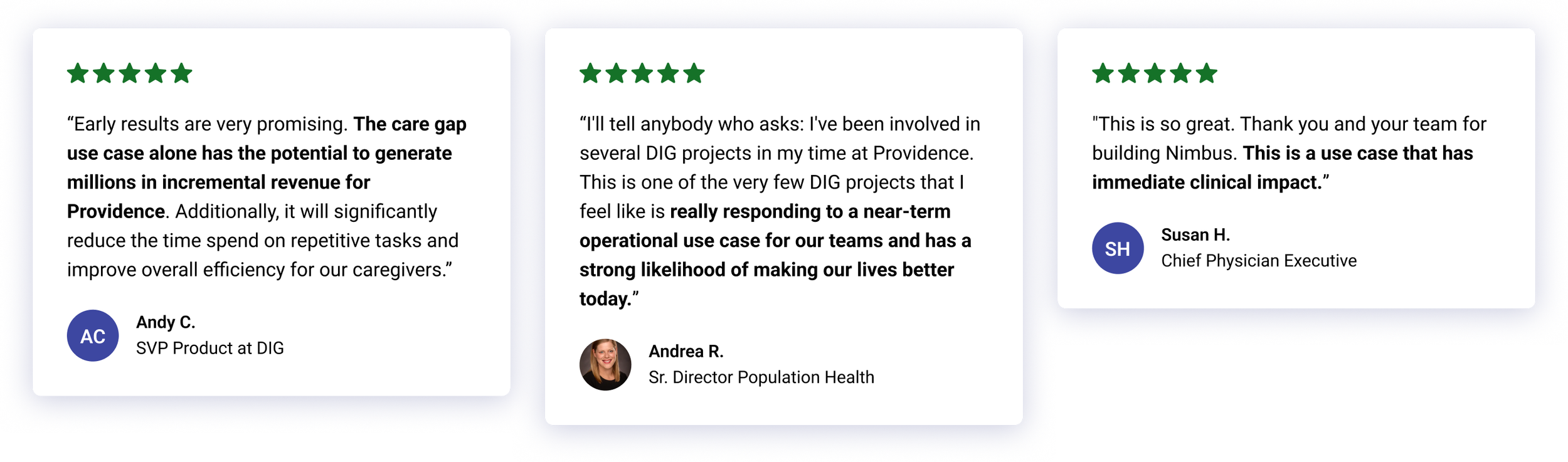
user satisfaction
Gaining executive buy-in by showing measurable impact
We consulted caregiver teams throughout all stages of discovery, design, and development. The co-design process helped us establish trust and turned key stakeholders into strong advocates. Positive feedback combined with early promising results from our Proof of Concept enabled the project to gain buy-in from key executives at Providence.